Connect With Us

Symptoms of Peripheral Artery Disease

Peripheral artery disease, also known as PAD, can manifest with a range of symptoms. Roughly half of individuals with PAD experience typical symptoms. Others may have atypical or no symptoms at all. Regardless of the presence or absence of symptoms, individuals with PAD face an increased risk of cardiovascular disease. Left untreated, PAD can lead to serious complications, such as ulcers and infections. Common signs of PAD are intermittent pain, aching, heaviness, or cramping in the legs during activities such as walking or climbing stairs. This discomfort typically subsides with rest and is often felt in the calf but can also occur in the buttocks, thigh, or foot. Additionally, PAD may lead to changes in toenails and leg hair growth, with one foot possibly feeling colder than the other. The affected leg or foot may appear pale, discolored, or even blue. Some individuals may experience leg weakness or numbness, making walking more challenging, and report sensations like pins and needles. In severe cases, blockage of blood flow can result in pain even at rest. Advanced PAD can cause sores or wounds on the toes, feet, or legs, which may heal slowly or not at all and are prone to infections. These symptoms emphasize the importance of scheduling an appointment with a podiatrist for early detection and prompt treatment to manage PAD effectively and reduce the risk of complications.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. David Ungar from Personal Foot Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Farmington, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
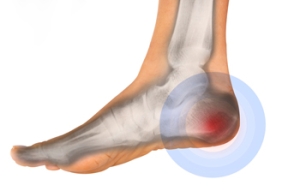
Various Causes of Heel Pain
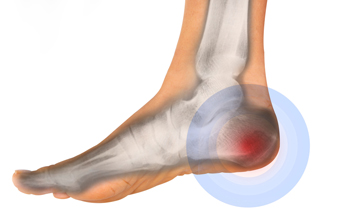
Heel pain, a pervasive discomfort impacting daily activities, can be attributed to a myriad of factors. Plantar fasciitis, a common cause, arises from inflammation of the plantar fascia, the tissue connecting the heel bone to the toes. Excessive strain on this ligament, often from overuse or wearing improper footwear, can lead to stabbing pain. Achilles tendonitis, inflammation of the Achilles tendon at the back of the heel, contributes to discomfort, particularly in activities that stress the calf muscles. Additionally, heel spurs, bony protrusions at the bottom of the heel, may result from prolonged plantar fasciitis, causing intermittent or chronic pain. Other potential causes may include stress fractures, nerve impingement, or bursitis. Foot anatomy, gait abnormalities, and excessive weight can further exacerbate heel pain. Identifying the specific factors that contribute to heel pain is essential for tailored interventions. If you have heel pain, it is strongly suggested that you are under the care of a podiatrist who can determine the cause and offer appropriate treatment methods.
Many people suffer from bouts of heel pain. For more information, contact Dr. David Ungar of Personal Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Farmington, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
Ingrown Toenails and Infection Control

Ingrown toenails, a common condition where the nail grows into the toe's skin, can lead to infections if not properly managed. They most often affect the big toe and can result from trauma, improper nail trimming, and wearing tight footwear. The skin surrounding the ingrown nail becomes red, swollen, and painful, and may produce pus, indicating an infection. Preventing infection in ingrown toenails involves proper foot hygiene and nail care. Toenails should be cut straight across, avoiding rounding the corners which can encourage the nail to grow into the skin. Wearing properly fitting shoes that provide enough space for the toes to wiggle freely in can also reduce the risk. If you have an ingrown toenail and suspect an infection, it is strongly suggested that you make an appointment with a podiatrist for an evaluation and treatment.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Dr. David Ungar of Personal Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Farmington, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ingrown Toenail Care
An ingrown toenail is a toenail that grows sideways into the nail bed, causing pain and swelling. Ingrown toenails can worsen and cause drainage, turning into a serious infection.
Several factors affect whether a person is at risk from an ingrown toenail. The many causes include being overweight, diabetes, participating in sports, having a fungal infection of the toe, and cutting your nails too short. Ingrown toenails also have a genetic predisposition, causing some people to be more prone to receive the condition than others. Other causes include improperly fitting shoes and shoes that keep the feet damp.
Ingrown toenails can be preventable with certain measures. For starters, allowing your toe nails to grow slightly longer in length will help prevent them from becoming ingrown. If you have already developed an ingrown toenail, soak the affected toe in warm water. This will alleviate the pain and help prevent an infection from forming. Antibiotic soap or Epsom salts may be added to further help the relieving process and avoid infection. Placing cotton beneath the affected area is also suggested, as this may help the toenail grow upwards and not into the nail bed. Swelling and redness can be reduced by resting with your feet elevated.
A podiatrist should be seen if the pain becomes so serious that it prevents you from doing your everyday activities. If a red streak running up your leg appears or if you suspect your infection has spread, contact a podiatrist immediately. Fast treatments can be undertaken to lessen your pain and have you walking comfortably.
An ingrown toenail can be easily treated with a Band-Aid. Simply wrap the affected toe with a Band-Aid to prevent infection and keep the nail from growing out at a painful angle.
In more serious cases, your podiatrist may decide to make a small incision to remove a portion of your toenail. To prevent the nail from growing back, medication will be placed directly into the nail bed. This procedure would be performed under local anesthesia and is a faster method to alleviate discomfort from an ingrown toenail. Post-procedure directions will have you stay off the affected foot for a day. Afterwards, normal activities can be resumed.
Diabetes and Its Impact on Foot Health

Diabetes, a chronic condition affecting blood sugar levels, can significantly impact the health of your feet. Elevated blood sugar levels can lead to nerve damage, a condition known as diabetic neuropathy. As a result, individuals with diabetes may experience reduced sensation in their feet, making it challenging to detect injuries or infections. Poor circulation, another common consequence of diabetes, can slow down the healing process, increasing the risk of complications. Foot ulcers, a prevalent issue among those with diabetes, can develop from minor injuries or pressure points. Left untreated, these ulcers may lead to severe infections. Regular foot inspections, meticulous hygiene, and wearing proper footwear are crucial for preventing complications. It is important for Individuals with diabetes to prioritize foot care as an integral part of their overall health management, seeking prompt medical attention for any concerning symptoms to maintain optimal foot health. If you have diabetes, it is strongly suggested that you schedule regular appointments with a podiatrist who can help you to manage this condition.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dr. David Ungar from Personal Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Farmington, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes affects millions of people every year. Blood vessels located all over the body are damaged due to diabetes—even the blood vessels of the feet. Neuropathy, or nerve damage, can result from slower blood flow in the legs and feet. In diabetic patients, neuropathy is very important to monitor, as diabetics are at risk for developing ulcers.
Always washing and thoroughly drying the feet are pertinent parts of diabetic foot care. There should be a focus on cleaning between the toes. Even if no pain is felt, the entire foot should be examined for redness and sores. Neuropathy can often mask the pain of sores and ulcers and can cause these conditions to be overlooked. Use a mirror to examine the underside of your feet if needed. It is recommended that diabetics wear well-fitting socks.
Patients with diabetes should have their doctor monitor their blood levels because blood sugar levels play a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised. It is very important to keep your blood sugar levels in the normal range, which can be determined by your physician. There are medications that may be prescribed to help with any neuropathy experienced by the diabetic patient. It is also advisable to visit a podiatrist if one is experiencing any conditions involving the feet, such as ingrown toenails, which in more severe cases can cause infection.
Diabetic feet must be inspected daily. Diabetic foot care at home is possible if a patient is provided with instructions from their podiatrist. Patients can relieve dry heels with creams or ointments. Suspected wounds should warrant an immediate call to the podiatrist. Gangrene is a serious problem for diabetics and can lead to sepsis and amputation in its worst cases. Early treatment and daily inspection of diabetic feet are keys to staying healthy.
Negative Effects of Wearing High Heels

Many people love wearing stilettos but certainly not the pain that comes with them. The repercussions of wearing high heels extend beyond aching feet. According to experts, consistently wearing the wrong type of heels can take a toll on your feet, ankles, knees, and back. The pressure on the forefoot intensifies as you elevate the heel, leading to metatarsalgia, a painful joint condition in the ball of the foot. Chronic metatarsalgia can result in stress fractures. Research indicates that reducing heel height can significantly alleviate foot pressure. While three inch heels place 76 percent of the weight on the forefoot, opting for two inch heels decreases it to 57 percent, and one inch heels further reduce it to 22 percent. The Achilles tendon, vital for foot movement, faces strain as wearing high heels may cause excessive shortening. This stress can extend to the plantar fascia, resulting in plantar fasciitis, a painful condition that affects the heel and arch. In addition, studies show that initial ankle muscle strengthening from wearing heels regularly diminishes over time, leaving women susceptible to the risk of falls and ankle sprains. For help with managing foot and ankle problems caused by wearing high heels, it is suggested that you schedule an appointment with a podiatrist.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact Dr. David Ungar from Personal Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
- Ankle Joints
- Achilles Tendon – May shorten and stiffen with prolonged wear
- Balls of the Feet
- Knees – Heels cause the knees to bend constantly, creating stress on them
- Back – They decrease the spine’s ability to absorb shock, which may lead to back pain. The vertebrae of the lower back may compress.
What Kinds of Foot Problems Can Develop from Wearing High Heels?
- Corns
- Calluses
- Hammertoe
- Bunions
- Morton’s Neuroma
- Plantar Fasciitis
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions please feel free to contact our office located in Farmington, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Effect of High Heels on the Feet
High heels are uncomfortable, but many women sacrifice comfort to be stylish. There are many problems that stem from wearing high heels, however these issues can be avoided by wearing proper shoes.
Heels are bad because they push your weight forward toward the fall of the foot. The higher the heel is, the more weight and pressure get shifted. This process causes the back to hyperextend backwards to counterbalance which may cause pain in the leg, hip, and back. Consequently, major posture problems may occur, and these issues may eventually become permanent.
Wearing high heels is one of the leading cause of ingrown toenails. Heels create a great deal of pressure on the big toenails which disrupts proper toenail growth. This may eventually lead to the big toenail growing into the skin. Another common problem that stems from high heels is bunions. If bunions go untreated, they can cause serious scar tissue to form along with severe pain.
However, there are ways to minimize the harmful risks associated with wearing heels. You should try to massage and stretch your legs and feet after wearing heels for an extended time. Stretching helps prevent the Achilles tendons and calf muscles from becoming too tight. A good substitute for heels are platforms which provide a better surface area to evenly distribute the body’s weight.
If you are experiencing any painful foot conditions from wearing high heels, you should consult with your podiatrist right away.